Chronic pain affects approximately 100 million US adults, and has devastating consequences on quality of life (QoL) and functional status.1 Unfortunately, despite the availability of various pharmacologic and nonpharmacologic therapies, many patients with chronic noncancer pain continue to experience moderate or severe symptoms.1
Numerous barriers exist to the optimal management of pain, including patients’ hesitation to address pain; patients’ difficulty in communicating their pain symptoms; a lack of knowledge of, and access to, the available pain treatment options; provider attitudes and training; the underutilization of effective prescription medications, such as opioids; the inability to pay for pain treatment or a lack of insurance coverage; and the underestimation of the impact of chronic pain on patient well-being by all the stakeholders.1 Systematic efforts to understand and to eliminate the barriers to effective pain control are essential, and need to be an integral part of patient care, particularly in disease conditions that predispose individuals to pain.
This article addresses efforts for improving the quality of pain care through the support of prescriber and patient education; effective and targeted advocacy initiatives; and collaborative efforts by regulatory bodies, policymakers, healthcare providers, and patient advocacy groups.
Focus on Provider, Patient, and Public Education
Despite the widespread prevalence of chronic pain in the United States and the enormous demands on patient well-being and healthcare costs, there is a lack of awareness of the magnitude of this socioeconomic burden and of the need for effective pain management across the stakeholders.1 As a result, healthcare providers, patients, legislators, payers, and society as a whole are not adequately prepared to recognize or to initiate appropriate and timely treatments; these deficiencies in knowledge, competency, and awareness among each of the stakeholders must be addressed to achieve the optimal management of pain.1 Therefore, the Institute of Medicine (IOM) recognizes that education is necessary to transform the understanding of pain.1
Particularly, opioid prescription use remains highly controversial, even in the wake of treatment guidelines and educational efforts among all stakeholders, largely stemming from fear of drug abuse and medication misconceptions.1 It is critical to increase understanding that better and timely treatment of acute pain may avoid the progression to chronic pain, which is more difficult and expensive to treat.1
Provider Education
As evidenced by reports of a lack of competency in physician pain training, the underestimation of pain prevalence and its impact on patients’ QoL, and a lack of adherence to pain management guidelines by healthcare providers, there is widespread concern that current knowledge about pain management is not being optimally applied in clinical practice, resulting in delayed and inadequate pain care.1 Specifically, knowledge gaps have been identified in several opioid-related areas, including the appropriate use of prescription opioids for chronic noncancer pain; misconceptions about the abuse potential of opioids; illegal diversion; adverse effects of opioids; and patient-related issues, such as medication nonadherence, psychiatric comorbidity, and secondary gain.1-3 For these reasons, opioid prescription use remains highly controversial.
Furthermore, evidence indicates that physicians are nonadherent to chronic pain management guidelines; 1 survey study reported that the majority of primary care physicians were noncompliant with evidence-based Agency for Healthcare Research and Quality’s guidelines for the initial management of chronic low back pain.1,4 Clearly, programs are needed to educate healthcare providers about pain management approaches, including the appropriate use of opioids.
In this context, studies that used surveys to assess the concerns, perceptions, and practices of medical providers revealed that nearly 72% of physicians considered their knowledge of treatment and management of opioid dependence as being low. Furthermore, the surveyed medical providers evaluated their own medical training in this area as unsatisfactory.3 These data are consistent with accumulating evidence that indicates that pain education in US medical schools is inadequate, variable, and fragmented.1,5
A recent study of 117 US and Canadian medical schools found that 80% of US medical schools require only ≥1 pain sessions. These courses are not specialized; they are typically presented as part of general required courses, and do not cover the topics included in the International Association for the Study of Pain core curriculum.5
Furthermore, the First National Pain Medicine Summit of 2009 reported an inconsistency in teaching across medical schools, a limited scope of topic, a lack of integration of basic science and clinical knowledge, and a lack of clinical role models in the majority of academic medical centers.6
In addition, the American Board of Medical Specialties does not recognize pain medicine as a separate physician specialty but rather as a subspecialty fellowship training program that is offered by anesthesiology, physical medicine and rehabilitation, psychiatry, and neurology residency programs.1 There is now growing support for the development of a separate pain care specialty that is not under the aegis of any medical discipline, which is expected to promote a greater continuity of care than is currently the status quo.1
Because there is a shortage of pain specialists in the United States, the primary care practitioner is the main pain care provider for the majority of patients with common chronic pain problems.1 However, primary care physicians report that they are ill-prepared and lack the confidence to adequately manage patients with pain&emdash;underscoring the urgent need for pain education for these professionals who are at the frontlines of care.7,8 According to the IOM, recognizing pain management as part of the core competency of internal medicine can substantially improve the practice of pain medicine by primary care physicians.1
Clearly, there is a need for better integration of pain topics into medical school curricula, development of a uniform process for training and certification, and pain medicine education for primary care physicians. In support of this view, the key recommendations of the IOM are to expand education programs to transform the understanding of pain; improve curriculum and education for healthcare professionals; and increase the number of healthcare professionals with advanced expertise in pain care.1
In addition, many physicians do not dedicate sufficient time to listen to patients’ complaints.1,9,10 Such pain apathy prevents these professionals from providing pain care and may be rooted in feelings of negative emotions, such as frustration and guilt over their ability to treat chronic pain, as well as deficits in provider–patient communication, inadequate knowledge, limited previous experience with analgesic use, uncertainty about the veracity of reported pain, and an absence of objective or physiological measures of pain intensity.2,9,10
One study that explored physicians’ communications with patients with cancer pain found that physicians did the majority of the talking during the visits and interrupted patients’ attempts to provide information or ask questions, all of which may have deterred patients from revealing their pain experience.11 Therefore, communication skills of the healthcare provider, including demonstrating empathy and encouraging shared decision-making, is another area in need of improvement.
Patient Education
Patient education is integral to effective pain management because individuals with chronic pain often do not seek help, are unaware of their treatment options, and have misconceptions about pain management.1 Patient education has been reported to reduce the symptoms of chronic pain, and to improve functioning and overall QoL.1,12-14
Findings from 1 study showed that a physiotherapist-driven education intervention in patients with chronic low back pain demonstrated a strong relationship between cognitive change and improvements in physical functioning.14 In another study, behavioral training of patients with migraine by lay trainers with migraine resulted in significant reductions in attack frequency and in the improvement of QoL, as well as feelings of control and self-confidence.13
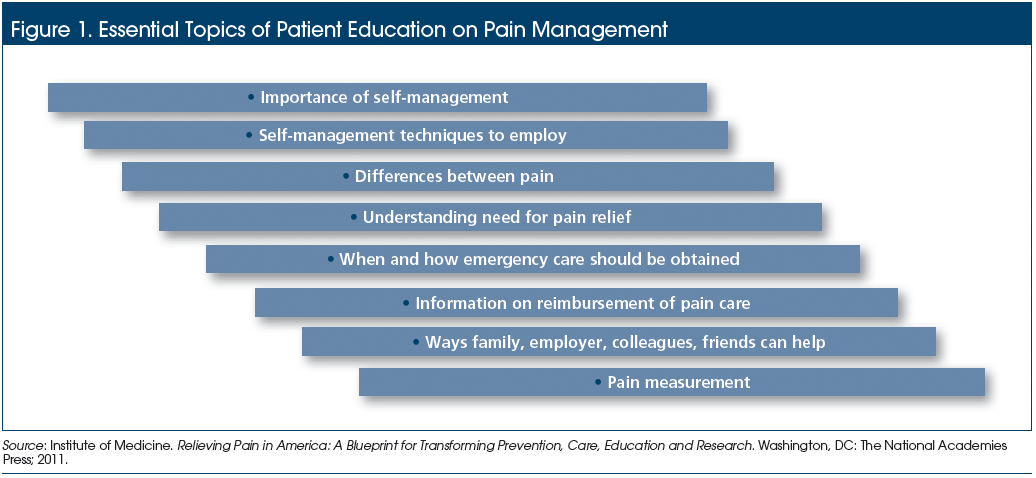
Essential topics of patient education include the prevention of common types of pain, the importance of self-management, when and how to obtain urgent care, understanding the need for pain relief, available treatment options, treatment goals, access to other resources and support, and pain measurement (Figure 1).1 Self-management is an essential component of pain care, and serves as a means to empower patients, with the goals of preventing or obtaining relief, preventing acute pain from progressing to chronic pain, and preventing chronic pain conditions from worsening.1
Results of a 1-year randomized controlled clinical trial in patients with arthritis and fibromyalgia showed that those who used an Internet-based arthritis self-management program as an educational intervention achieved significant improvements in self-efficacy and health status measures compared with patients who received usual care.15 Consistent with these reports, a meta-analysis of 17 arthritis self-management education programs supported the clinical effectiveness of patient education in reducing pain and disability.16 In particular, the benefits of psychosocial education in pain management has been demonstrated. Results from a randomized study showed that such interventions in a primary prevention setting improved knowledge about low back pain and the ability to cope with this condition compared with no education.17
However, available evidence indicates that patients with chronic pain do not receive timely, appropriate, and effective education.1 This is exemplified by survey findings that approximately 50% of patients with chronic pain who visited an emergency department reported receiving information about pain treatment options or referrals to pain specialists, although >75% of those patients indicated that they would have liked to receive such information, suggesting a need for improved care in this area.18
The IOM recommends that the content, timing, and goals of patient education be tailored to the individual patients’ medical needs, with the educational format adapted to the education and literacy level, age, and cultural and linguistic needs of the patient.1 Such educational strategies must also be directed toward families and caregivers, because of their critical role in the effective management of chronic pain.
Public Education
An essential component of the 10 Essential Public Health Services provided by public health systems is to “inform, educate, and empower people about public health issues.”19 The IOM identified 5 major reasons why public education about pain is essential.1 First, informed individuals are equipped to take steps to avoid pain (eg, practicing proper stretching and lifting techniques), and can adopt timely and appropriate self-management strategies when needed. Second, educated individuals can give appropriate advice and assistance to family members, friends, and others with pain, particularly by urging them to seek help when needed and not bear the pain; in addition, they can help to dispel common misconceptions about opioid medications. Third, educated individuals can seek appropriate chronic pain treatment for themselves or their family members. Fourth, an educated public can help to minimize hazards that contribute to pain-producing injuries among students and in the general community. Finally, an educated community can advocate for improved pain prevention and control policy measures (eg, lawful access to medically necessary opioid medications, health insurer reimbursement of interdisciplinary pain care).1
Public education is critical for fostering relevant advocacy initiatives at the community level. The expertise developed by pain care advocates in the complexities of pain management allows to identify relevant issues to advocate for in an informed manner and make a positive impact on the overall management of pain.1
Role of Advocacy Measures
Although the clinical, economic, and societal burdens of pain are substantial and represent a public health crisis, chronic pain has been largely omitted from the current national debate on health reform.20 Therefore, it is imperative that policymakers are made aware of the huge impact of chronic pain on the nation’s social and economic well-being, and prioritize to develop and to implement appropriate and timely interventions to curb its tide.20 From a policy perspective, there is a need for “whole systems approaches within a culture of collaboration across all stakeholders.”20
According to the IOM, “effective, multifaceted, and coordinated advocacy is a necessary condition for cultural transformation,” and such efforts require the “combined voice of a strong coalition” in order to make a significant impact on key stakeholders at the federal, state, and key private organization levels.1 One successful advocacy program is the Massachusetts Pain Initiative, which has supported state legislation that mandates pain assessment and management in all healthcare facilities, requires pain management and prescription drug abuse training for all clinicians, and establishes a prescription monitoring program task force.21
In the current value-driven healthcare delivery landscape, an important area of advocacy is to improve reimbursement policies. The lack of insurance coverage is a major contributor of the observed disparities in the delivery of pain care, and an inability to pay for pain care is particularly prevalent among minorities and women.22 Furthermore, despite the established benefit of psychosocial services and interdisciplinary approaches to pain management, many patients with insurance coverage are faced with restrictions on such services or on the frequency of physician visits.1
Collaborative Efforts
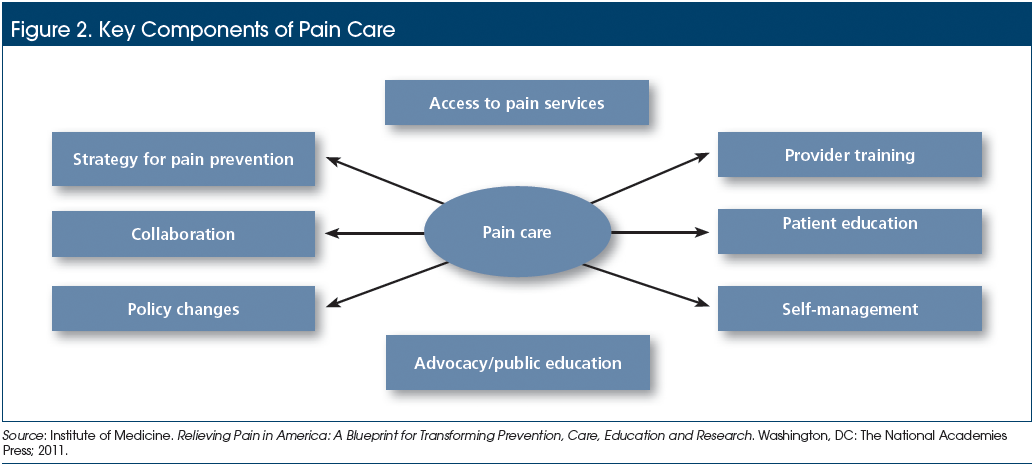
The 2011 IOM recommendations support the establishment of an interdisciplinary team for the delivery of optimal pain management (Figure 2).1 An integrated, coordinated, and multimodal approach would address the different aspects of chronic pain management, including the reduction in pain severity, improved functioning, emotional well-being, and improvement in QoL.1 These goals may be accomplished through the adoption of interdisciplinary modalities, including pharmacologic, physiotherapy, psychologic, rehabilitation, and interventional approaches. The development of such a comprehensive program requires collaboration among multiple specialists, including pain specialists, primary care physicians, psychologists, rehabilitation specialists, and/or complementary and alternative medicine therapists.1
The effectiveness of an interdisciplinary team approach for pain management is well-documented.23,24 In the primary care setting, a multicenter, randomized, controlled clinical trial demonstrated that the implementation of a cognitive behavioral interventional strategy resulted in the improvement of pain and disability outcomes and was cost-effective in managing subacute and chronic low back pain.23 Furthermore, a Department of Veterans Affairs intervention (known as assistance with pain treatment) that was led by a psychologist care manager and an internist, reduced pain among primary care patients through clinician and patient education, assessment, symptom monitoring, feedback to clinicians, and referrals to specialists.24
Alternatively, a strong referral network or access to pain centers that are focused on providing interdisciplinary pain care also allows primary care physicians to access multimodal treatment resources for consultation or for the referral of patients with severe or recalcitrant pain.1 Although outcomes data regarding effectiveness of pain centers are limited, available evidence supports the benefits of interdisciplinary care. For example, outcomes data show that patient care that is provided by pain centers is more beneficial than surgery for patients with back pain. Such data are particularly compelling, because patients who are referred to pain centers typically have a long history of chronic pain that has not responded to other treatments.25
Conclusion
There is an urgent need for education and training of healthcare providers, patients, and the public at large, in addition to collaboration among all stakeholders, including policy makers, to provide optimal pain care. Integrated care approaches that incorporate pain assessment, appropriate interventions, research for more effective treatments, advocacy for better policy changes, and effective education can optimize health outcomes in patients with chronic pain.
References
- Institute of Medicine. Relieving Pain in America: A Blueprint for Transforming Prevention, Care, Education and Research. Washington, DC: The National Academies Press; 2011. http://books.nap.edu/openbook.php?record_id=13172&page=17. Accessed December 12, 2014.
- Barry DT, Irwin KS, Jones ES, et al. Opioids, chronic pain, and addiction in primary care. J Pain. 2010;11:1442-1450.
- Keller CE, Ashrafioun L, Neumann AM, et al. Practices, perceptions, and concerns of primary care physicians about opioid dependence associated with the treatment of chronic pain. Subst Abus. 2012;33:103-113.
- Webster BS, Courtney TK, Huang YH, et al. Physicians’ initial management of acute low back pain versus evidence-based guidelines. Influence of sciatica. J Gen Intern Med. 2005;20:1132-1135.
- Mezei L, Murinson BB. Pain education in North American medical schools. J Pain. 2011;12:1199-1208.
- Lippe PM, Brock C, David J, et al. The first national pain medicine summit—final summary report. Pain Med. 2010;11:1447-1468.
- O’Rorke JE, Chen I, Genao I, et al. Physicians’ comfort in caring for patients with chronic nonmalignant pain. Am J Med Sci. 2007;333:93-100.
- Upshur CC, Luckmann RS, Savageau JA. Primary care provider concerns about management of chronic pain in community clinic populations. J Gen Intern Med. 2006;21:652-655.
- Notcutt W, Gibbs G. Inadequate pain management: myth, stigma and professional fear. Postgrad Med J. 2010;86:453-458.
- Dobscha SK, Corson K, Flores JA, et al. Veterans affairs primary care clinicians’ attitudes toward chronic pain and correlates of opioid prescribing rates. Pain Med. 2008;9:564-571.
- Berry DL, Wilkie DJ, Thomas CR Jr, et al. Clinicians communicating with patients experiencing cancer pain. Cancer Invest. 2003;21:374-381.
- Albaladejo C, Kovacs FM, Royuela A, et al. The efficacy of a short education program and a short physiotherapy program for treating low back pain in primary care: a cluster randomized trial. Spine (Phila Pa 1976). 2010;35:483-496.
- Merelle SY, Sorbi MJ, van Doornen LJ, et al. Lay trainers with migraine for a home-based behavioral training: a 6-month follow-up study. Headache. 2008;48:1311-1325.
- Moseley GL. Evidence for a direct relationship between cognitive and physical change during an education intervention in people with chronic low back pain. Eur J Pain. 2004;8:39-45.
- Lorig KR, Ritter PL, Laurent DD, et al. The internet-based arthritis self-management program: a one-year randomized trial for patients with arthritis or fibromyalgia. Arthritis Rheum. 2008;59:1009-1017.
- Warsi A, LaValley MP, Wang PS, et al. Arthritis self-management education programs: a meta-analysis of the effect on pain and disability. Arthritis Rheum. 2003;48:2207-2213.
- George SZ, Teyhen DS, Wu SS, et al. Psychosocial education improves low back pain beliefs: results from a cluster randomized clinical trial (NCT00373009) in a primary prevention setting. Eur Spine J. 2009;18:1050-1058.
- Todd KH, Cowan P, Kelly N, et al. Chronic or recurrent pain in the emergency department: national telephone survey of patient experience. West J Emerg Med. 2010;11:408-415.
- CDC. 2011. National public health performance standards program. www.cdc.gov/nphpsp/essentialServices.html. Accessed December 12, 2014.
- Phillips C, Main C, Buck R, et al. Prioritising pain in policy making: the need for a whole systems perspective. Health Policy. 2008;88:166-175.
- Massachusetts Pain Initiative. 2011. Legislative issues and access to care council. http://masspaininitiative.org/index.cfm?p=p.12&title=Councils. Accessed December 12, 2014.
- Green CR, Hart-Johnson T, Loeffler DR. Cancer-related chronic pain: examining quality of life in diverse cancer survivors. Cancer. 2011;117:1994-2003.
- Lamb SE, Hansen Z, Lall R, et al. Group cognitive behavioural treatment for low-back pain in primary care: a randomised controlled trial and cost-effectiveness analysis. Lancet. 2010;375:916-923.
- Dobscha SK, Corson K, Perrin NA, et al. Collaborative care for chronic pain in primary care: a cluster randomized trial. JAMA. 2009;301:1242-1252.
- Boris-Karpel S. Policy and practice issues in pain management. In: Ebert MH, Kerns RD, eds. Behavioral and Psychopharmacologic Pain Management. New York, NY: Cambridge University Press; 2010.
